Sleep disturbances in older adults with mild cognitive impairment

- By Simon Beaulieu-Bonneau
- 21-August-2009
Abstract
Background: Normal aging and dementia are characterized by an increased prevalence of sleep disorders and alterations of both sleep continuity and architecture. However, little is still known about the nature of sleep in mild cognitive impairment (MCI), which is presumably situated on the continuum from healthy aging to dementia. This unsystematic review summarizes the current literature on the prevalence and severity of sleep disturbances in MCI.
Methods: Eighteen studies addressing sleep/night-time disturbances among other neuropsychiatric symptoms in individuals with MCI were identified through a search of databases and an examination of reference lists of selected papers. Fifteen of those studies reported data on the prevalence or severity of sleep/night-time disturbances.
Results: Results indicated that 14-59% of patients with MCI had sleep disturbances. These disturbances were often identified as one of the four most prevalent neuropsychiatric symptoms of MCI and were considered clinically significant in some studies. In addition, there was some evidence that the prevalence of sleep disturbances in MCI is intermediate between that of normal aging and dementia. Longitudinal data suggest that sleep problems are associated with both incident MCI and dementia.
Conclusions: These findings support the hypothesis that sleep disturbances are one of the core non-cognitive symptoms of MCI. It remains to be known whether sleep problems could help to identify those individuals with MCI who will eventually develop dementia. Studies characterizing sleep more systematically are needed to verify this proposition and to clarify the associations between sleep disturbances and other neuropsychiatric symptoms of MCI.
Background
Cognitive impairment is a general term for the loss of memory and other mental abilities, with Alzheimer’s disease (AD) being the most common cause of cognitive impairment. β-amyloid (Aβ) deposition in the brain is the main pathological change of AD, and the imbalance of production and clearance of Aβ is the main reason Mild Cognitive Impairment (MCI) describes a state of cognitive functioning that is below defined norms, yet falls short of dementia in severity, which exists across a cognitive continuum with borders that are difficult to define precisely Sleep is an important physiological process and is conducive to the elimination of brain metabolites and the recovery of brain function The restoration of brain function during sleep may be due to enhanced clearance of waste products, including Aβ, accumulated in waking moments in the central nervous system.
In recent years, emerging studies have explored the link between sleep and cognitive impairment, with the advancement of the world population aging. Short naps could mitigate the harmful effects of short sleep duration (the total sum of time spent asleep, regardless of sleep stage) on cognitive function. Sleep quality refers to one’s satisfaction with the sleep experience, integrating aspects of sleep initiation, sleep maintenance, sleep quantity, and refreshment upon awakening. Although poor sleep quality had a negative effect on mood and quality of life, sleep quality was not significantly independently associated with MCI in epilepsy. Obstructive sleep apnea (OSA) is characterized by episodes of a complete (apnea) or partial collapse (hypopnea) of the upper airway with an associated decrease in oxygen saturation or arousal from sleep. Cognitive impairment is highly prevalent in patients referred to sleep clinics for suspected OSA in older males. A polygenic score (PS) is an estimate of an individual’s genetic liability to a trait or disease, calculated according to their genotype profile. Higher PS was linked to longer sleep duration and was also associated with better performance in global cognition, fluid reasoning, speed of processing, and language, but not memory. In the sample of the elderly, mainly African Americans, changes in wakefulness after sleep onset were associated with poor cognitive function. Insomnia was defined as trouble falling and/or staying asleep. This can be short-term to last for a few days to a few weeks and for some, it can be chronic and last for more than a month. Narcolepsy refers to a syndrome clinically characterized by excessive daytime sleepiness and sleep attacks plus one or more auxiliary symptoms including cataplexy, sleep paralysis, and hypnagogic hallucinations. Restless leg syndrome is a disorder that causes an overwhelming urge to move legs, usually associated with unpleasant sensations, often during sleep and relieved by movement. In a cross-sectional study conducted in China, the associations between insomnia, narcolepsy, and cognitive impairment were identified, but the associations between OSA, restless leg syndrome, and cognitive impairment were not supported among community residents.
Additionally, associations between Rapid-Eye-Movement or Non-Rapid-Eye-Movement sleep behavior disorder and cognitive impairment were conflicted.
Existing studies have mainly focused on certain aspects of sleep, such as sleep duration, and habitual sleep efficiency. And the results are varied. Little research has used comprehensive and integrated scales to assess various aspects of sleep quality. Besides, the associations between cognitive impairment and wake-up time were less reported. Assessing sleep by monitoring over several days with devices such as polysomnography, is susceptible to environmental and psychological factors. Therefore, more research is needed to comprehensively evaluate sleep quality over a relatively long period. Moreover, most studies have been carried out in high-risk populations, such as epilepsy, Parkinson’s disease, and Hemodialysis. But because these populations might have symptoms of cognitive impairment and sleep disturbance, there will be probably a confounding factor for exploring the relationship between sleep and cognition. In this study, we investigated the relationships between sleep disturbance and MCI in a community population, after excluding the individuals who suffered from AD and other diseases that may influence cognitive function. And sleep quality was evaluated by using the Pittsburgh Sleep Quality Index (PSQI), which covers many aspects of sleep over a 1-month time interval.
Methods
Study Design and Population:
Participants were enrolled from a cross-sectional study conducted in a village in Xi’an, China, from January 3 to March 26, 2017. The village was randomly selected by the method of cluster sampling, and its population composition as well as the villagers’ lifestyles were similar to that of rural areas of Xi’an. The inclusion criteria were (1) over 40 years old, (2) willing to join, and (3) informed consent. The exclusion criteria were (1) suffered from AD and other dementias, cerebrovascular diseases, and other neurological conditions that may influence cognitive function (such as epilepsy, central nervous system infections, Parkinsonism, intracranial trauma, or surgery), (2) suffered from the climacteric syndrome, (3) failed to complete the Pittsburgh sleep quality index (PSQI) and the Mini-Mental State Examination(MMSE) or not finishing the clinical investigation, (4) had incomplete data.
The Medical Ethics Committee of the First Affiliated Hospital of Xi’an Jiao tong University approved this study, and informed consent was obtained from every participant. The enrolled subjects were first given a face-to-face structured interview for health status, medical history, and physical examination at the committee office or their own home if they had difficulties going to the office. Meanwhile, fasting blood samples of individuals were collected from 9 am to 11 am.
Cognitive assessment:
All the subjects were carried out a cognitive screening using the Mini-Mental State Examination (MMSE). The cutoff values were as follows: ≤17 for subjects with illiteracy, ≤ 20 for primary school-educated subjects, and ≤ 24 for those educated at the junior high school level or above. Participants with MMSE scores ≤ cutoff values underwent the 2nd phase cognitive examinations, including the Fuld Object Memory Evaluation test, Rapid Verbal Retrieval test, Trail-Making test, Digit Span test, and Block Design test. The diagnosis of MCI was determined according to the diagnostic criteria for MCI by a senior neurologist.
Assesses of Sleep Quality:
All subjects were asked to assess their sleep quality over a 1-month time interval by independently completing the Pittsburgh Sleep Quality Index (PSQI). PSQI is a self-rated questionnaire consisting of 8 parts(subjective sleep quality, wake-up time, sleep latency, sleep duration, habitual sleep efficiency, sleep interference, use of sleeping medication, and daytime dysfunction)and is obtained through 19 independent questions. Sleep efficiency is the ratio of the total time spent asleep (sleep duration) in a night compared to the total amount of time spent in bed. Sleep disturbance was defined as a PSQI score > 5.
Other covariates:
Participants self-reported sociodemographic variables (age, gender, and education level) and specific clinical factors (smoking and/or alcohol status), and disease variables (diabetes, hypertension, hyperlipidemia, anxiety, and depression). Participants also had a neurological examination, a systemic physical examination, blood biochemical examination. Body mass index (BMI) was calculated as weight divided by height squared and divided into four levels: underweight (BMI, < 18.5), normal weight (BMI, 18.5–23.9), overweight (BMI, 24-27.9), obese (BMI > 28). Smokers are defined as those who have smoked continuously or accumulated for 6 months or more during their lifetime. Drinking is defined as exceeding a certain daily drinking amount (e.g. 3 standard cups per day) or drinking amount per time (e.g. 5 standard cups per time, at least once a week). The diagnoses of diabetes, hypertension, hyperlipidemia, anxiety, and depression were based on self-reported disease history or taking anti-hypertensive, anti-diabetic, lipid-lowering drugs, anti-depressants, or anti-anxiety medications, or newly diagnosed according to guidelines.
Statistical analysis:
Histogram and normal probability plot of standardized residual, and residual plots were performed to ensure the normality and homogeneity of residuals. A comparison of approximately normal continuous variables was conducted by independent t-test and mean (SD). Mann-Whitney U test and median (interquartile range) were employed to compare the difference of the abnormal distributed continuous variables, and the χ2 test and number (percentage) were used to compare categorical variables.
The relationship between cognitive impairment and sleep disturbance was analyzed by simple Spearman’s correlation analysis first. Then, bivariate Logistic regression analysis was employed to adjust the confounding factors such as sociodemographic variables (age, gender, and education level), specific clinical factors (smoking and/or alcohol status, BMI), and disease variables (diabetes, hypertension, hyperlipidemia, anxiety and depression).
Next, using the same method to analyze the relationship between specific components of sleep disorder and MCI. All the analyses are two-sided. P < 0.05 was statistically significant. All statistical analyses were carried out using SPSS (IBM, USA,22.0 version). All of the graphs were drawn in GraphPad Prism (Texas,8.3.0 version).
Results
The Characteristics of the Study Population:
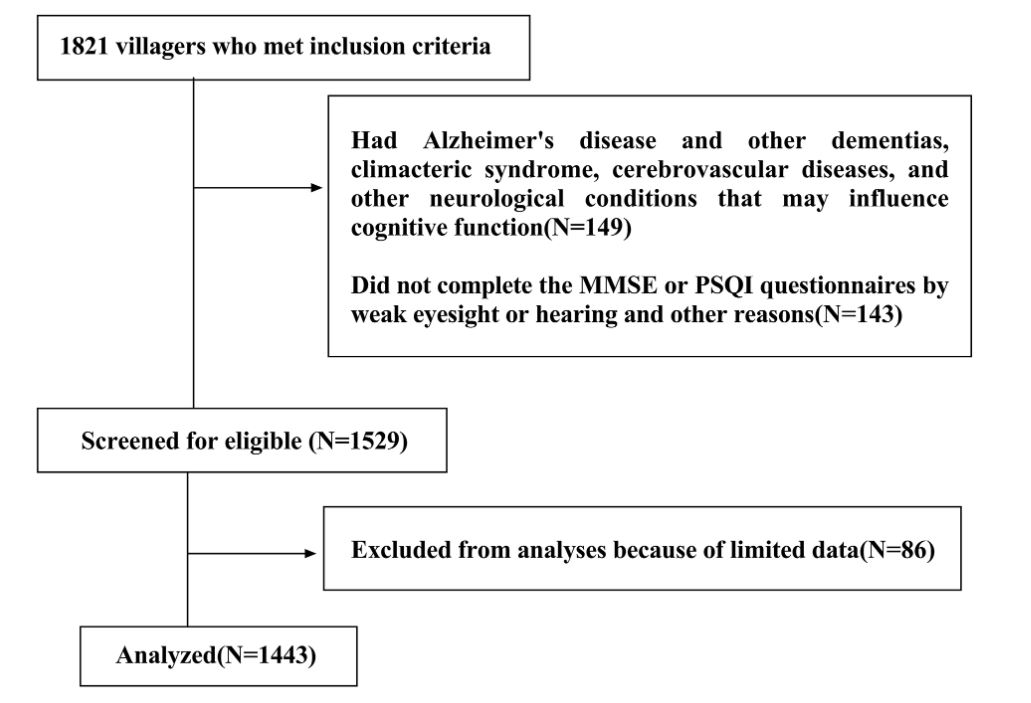
1,821 villagers met the inclusion criteria. Of these, 149 had Alzheimer’s disease and other dementias, climacteric syndrome, cerebrovascular diseases, and other neurological conditions that may influence cognitive function, 143 did not complete questionnaires, and 86 were excluded because of limited data. Finally, 1,443 were included in the analysis.
Fig. 1
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
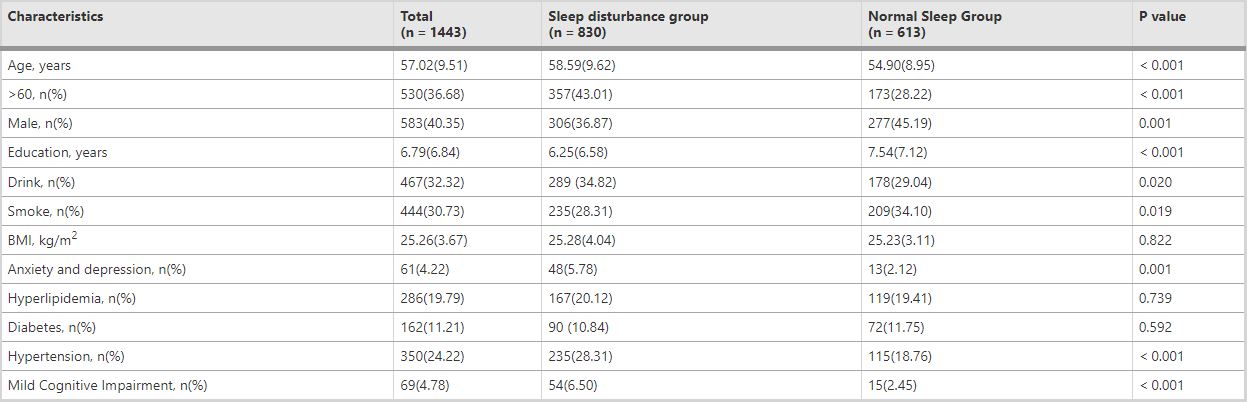
Among 1,443 participants, 830(57.52%) had sleep disturbance, and 69(4.78%) had cognitive impairment. Table 1 lists the clinical characteristics of the population. The total population is divided into normal sleep groups and sleep disturbance, according to sleep quality. Compared with the normal sleep group, the sleep disturbance group was older, had more female subjects, shorter years of education, and had higher rates of drinking, hypertension, anxiety, and depression but lower rates of smoking. The prevalence of MCI in the sleep disturbance group was higher than that in the normal sleep group (6.50% vs. 2.45%, P < 0.001).
Table 1 Characteristics of the total study population
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
The factors associated with mild cognitive impairment
According to the cognitive states, the total population is divided into the normal cognition group and the MCI group. Compared with the normal cognition group, the MCI group was older, had more female subjects, shorter years of education, and fewer smoking problems. Above all, the prevalence of sleep disturbance in the MCI group was higher than that in the normal sleep group (78.26% vs. 56.48%, P < 0.001) (Table 2).
Table 2 Comparison of sleep disturbance group and normal sleep group
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
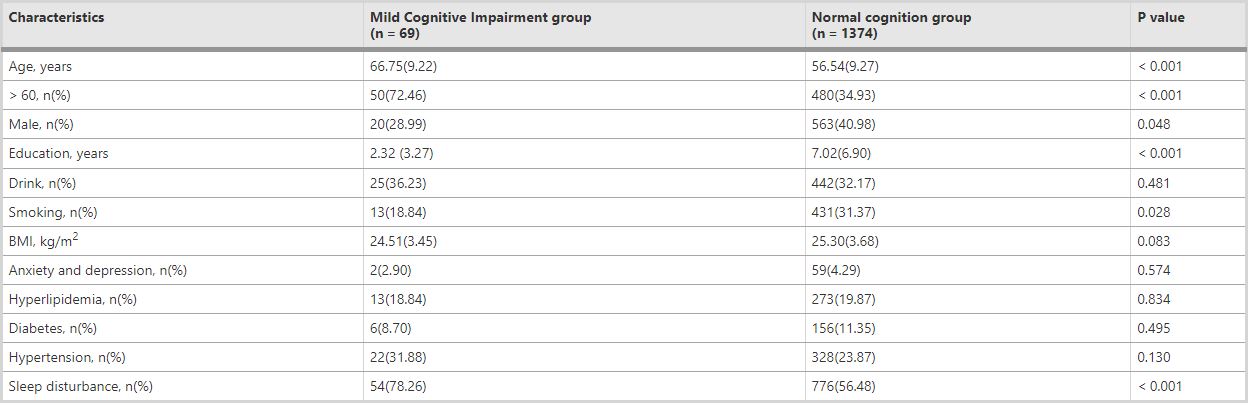
Table 3 Correlation analysis between cognitive impairment and clinical basic variables
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
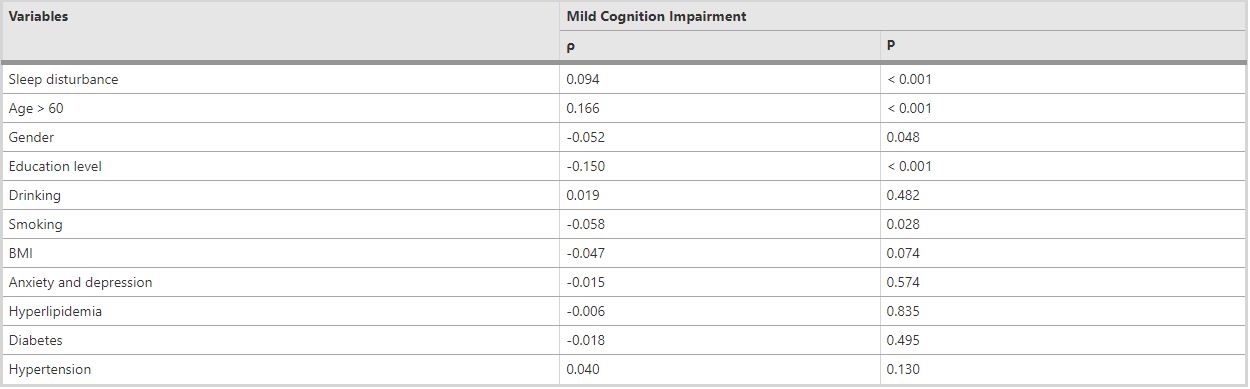
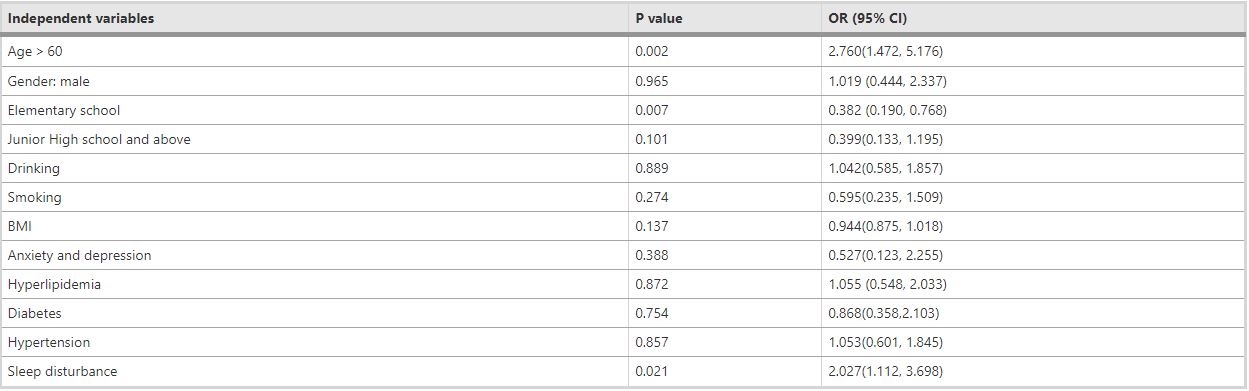
Table 4 Binary logistic regression of Mild Cognitive Impairment and clinical basic variables
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
The relationship between sleep disturbance and cognitive impairment
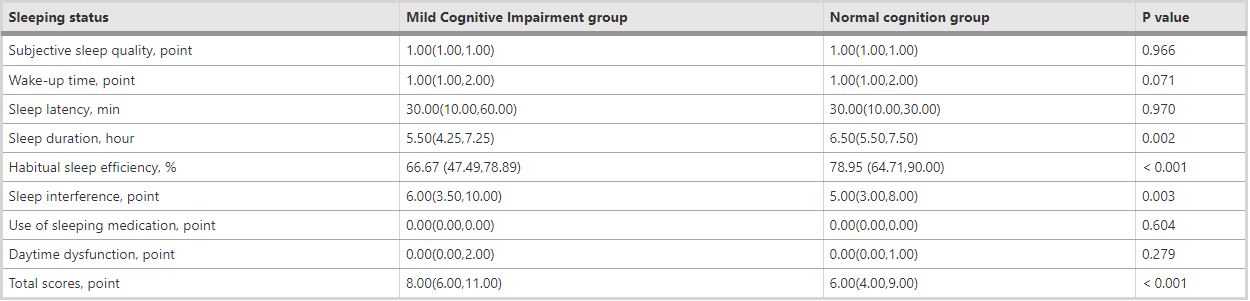
Compared to the normal cognitive group, the MCI group had a shorter sleep duration (5.5 h vs. 6.5 h, P = 0.002), lower habitual sleep efficiency (66.67% vs. 78.95%, P<0.001), and more sleep interference (6.0 points vs. 5.0 points, P = 0.003) (Table 5).
Table 5 Comparison of sleeping status in Mild Cognitive Impairment group and normal cognition group
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
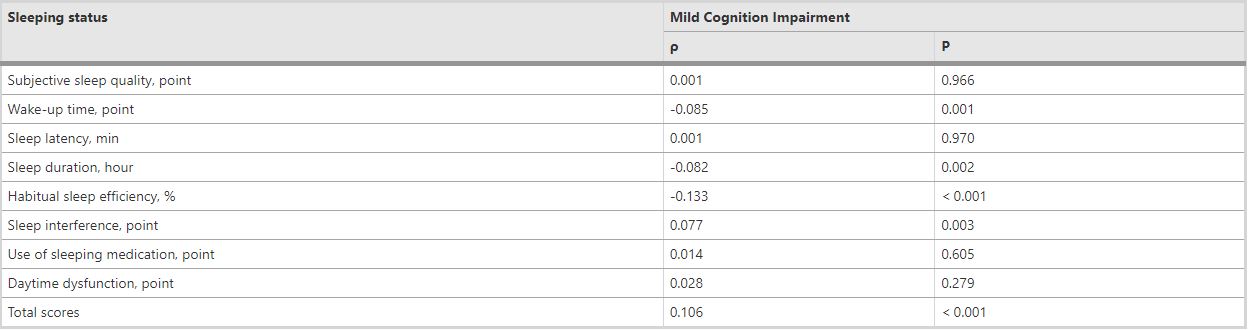
As shown in Table 6, MCI was positively correlated with Sleep interference (ρ = 0.077, P = 0.003), but negatively with Sleep duration (ρ=-0.082, P = 0.002), Wake-up time (ρ=-0.085, P = 0.001) and Habitual sleep efficiency (ρ=-0.133, P < 0.001).
Table 6 Correlation analysis of Mild Cognitive Impairment and internal components of sleep disturbance
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
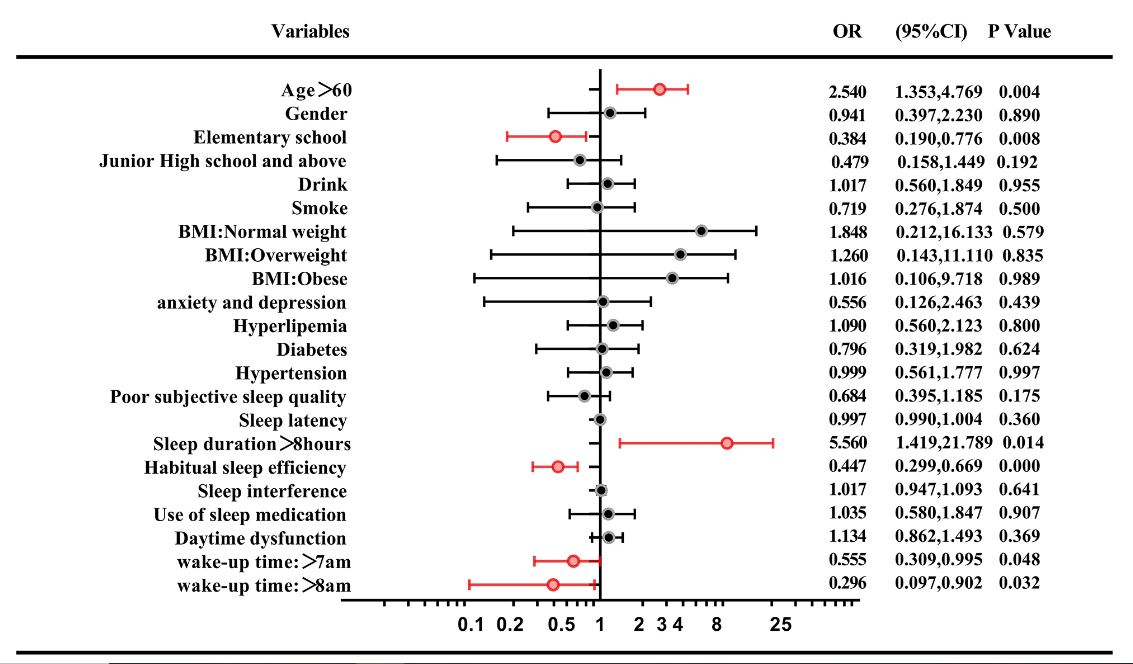
To further exclude the interference of other factors, the internal composition of sleep and other basic variables were included in the binary logistic regression. As shown in Fig. 2, MCI was still positively associated with the age>60 years old(OR = 2.540,95%CI = 1.353–4.769, P = 0.004), and negatively associated with the habitual sleep efficiency (OR = 0.447, 95%CI = 0.299–0.669, P < 0.001). MCI was negatively associated with waking up after 7 am (OR = 0.555, 95%CI = 0.309–0.995, P = 0.048), or 8 am (OR = 0.296, 95%CI = 0.097–0.902, P = 0.032), compared with waking up before or at 7 am. Besides, MCI was negatively associated with elementary school education level (OR = 0.384, 95%CI = 0.190–0.776, P = 0.008), compared with illiterate. In order to more accurately evaluate the effect of actual sleep duration on cognitive impairment, different sleep duration was included in the regression analysis in turn. It was found that MCI was positively associated with sleep duration of more than eight hours (OR = 5.560, 95%CI = 1.419–21.789, P = 0.014).
Fig. 2
From: Sleep disturbance is associated with mild cognitive impairment: a community population-based cross-sectional study
Discussion
In this population-based cross-sectional study, we used MMSE to assess cognitive function and used PSQI to evaluate sleep quality in more than 1,400 subjects. We found that MCI was positively associated with the age>60 years old, and negatively associated with the habitual sleep efficiency. People who slept more than 8 h a day might be more likely to suffer from cognitive impairment. Having an education level above illiteracy may reduce the risk of MCI. Moderately waking up later probably is beneficial to maintain normal cognitive function, which is different from what we previously thought, compared to waking up too early.
Compared to previous studies, the present study is a large sample, community population-based study. We used a method of random cluster sampling to select villages, and the population composition was similar to that in the rural areas of Xi’an which make the sample reasonably represent the rural areas of Xi’an. The diagnosis of cognitive impairment was made according to the MMSE score first, and then the subjects underwent the 2nd phase of cognitive examinations, to make sure the diagnosis of MCI reliable. Meanwhile, we used PSQI to assess sleep quality over a 1-month time interval. PQSI is a self-rated questionnaire, which assesses sleep quality and disturbances. The scale consists of 8 parts(subjective sleep quality, wake-up time, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction)and is obtained through 19 independent questions. PSQI score>5 yielded a diagnostic sensitivity of 89.6% and specificity of 86.5% (kappa = 0.75, P<0.001) for sleep disturbance. Eight indicators have proven that PSQI to be a reliable and effective measure of insomnia, with a Cronbach’s α of 0.83. These assure that our results are reliable and convincing.
Similar findings were found that sleep duration is positively associated with MCI risk, or in a U-shaped pattern. This association between longer sleep duration and an increased risk of MCI was also observed in Hemodialysis patients and adults with metabolic syndrome. However, some study shows short sleep duration is a risk factor for MCI, and there is a decreased risk of MCI for every additional hour of sleep among the elderly sleeping less than 7 h In this study, in order to more accurately evaluate the effect of actual sleep duration on cognitive impairment, different sleep duration was included in the regression analysis in turn, and after controlling for a variety of confounding factors, it was found that MCI may be more likely to occur if the sleep duration was more than eight hours.
Consistent with the findings of this study, several studies have suggested that habitual sleep efficiency is associated with MCI. Global cognitive performance is associated with sleep efficiency measured by polysomnography in patients with Parkinson’s disease. Compared to never reporting sleep difficulty, difficulty initiating sleep most nights was associated with worse cognitive function over time as was difficulty waking up too early most nights.
Subjects with cognitive decline exhibited lower sleep efficiency, and reduced inter-hemispheric connectivity during rapid eye movement sleep.
There are few studies on the relationship between wake-up time and MCI, which is a gap in sleep and cognition research. This study found that people who woke up at or after 7 am perhaps had a lower risk of MCI.
Although the exact mechanism of sleep disturbance involved in cognitive impairment has not been fully determined. A growing number of studies have found that sleep disorders may lead to cognitive impairment and accelerate AD pathology, including increased Aβ deposition in the brain our recent studies also showed that sleep deprivation-induced peripheral Aβ transport dysfunction in young adults, and Aβ accumulation in the brain in rats.
The underlying mechanism may involve the oxidative stress and inflammation.
Strengths
Compared with other studies with smaller sample sizes, this study was a large cross-sectional study with a sufficient study population and a well-representative population. We excluded 149 individuals who suffered from AD and other dementias, cerebrovascular diseases, climacteric syndrome, and other neurological conditions (such as epilepsy, central nervous system infections, Parkinsonism, intracranial trauma, or surgery) that may influence cognitive function. Moreover, we adjusted our analyses for other confounders, such as sociodemographic variables (age, gender, and education level), specific clinical factors (smoking and/or alcohol status), and disease variables (diabetes, hypertension, hyperlipidemia, anxiety and depression).
In this study, sleep quality was evaluated by using the Pittsburgh Sleep Quality Index (PSQI), which covers many aspects of sleep from subjective sleep quality, wake-up time, sleep latency, sleep duration, habitual sleep efficiency, sleep interference, use of sleeping medication, and daytime dysfunction. Assessing sleep quality with PSQI is more convenient and cost-effective, reflecting the usual sleep habits and quality without interference with the environment, thus allowing for assessing sleep quality in a large-sized study. Compared with the objective assessment of sleep quality, which was limited to a single night’s sleep, PSQI assesses sleep disturbances over a 1-month time interval.
The accuracy and reliability of the dependent variables were confirmed by the use of multiple cognitive scales and the final diagnosis of cognitive status by an experienced neurologist. Multiple covariates were included in binary logistic regression to eliminate the interference of numerous confounding factors to ensure the accuracy of our findings.
This study found that waking up before 7 am may be associated with an increased risk of MCI, which few studies have focused on before. In addition, this study also found that age over 60 years, illiteracy, lower sleep efficiency, and sleeping more than 8 h at night were associated with a higher risk of MCI. These findings will have important implications for the intervention of the risk of MCI and the prevention of dementia.
Limitations
Due to cross-sectional design, which prevents us from clarifying any causal and temporal relationship between cognitive impairment and sleep disturbance. A follow-up study to detect the changes in cognition function is necessary. On the other hand, we did not use any sleep monitoring devices to objectively assess sleep conditions, such as polysomnography and activity tracking, but relied on self-reporting, which may cause recall bias. However, studies have shown that the use of polysomnography to record the results of sleep in the elderly is consistent with subjective reports. In healthy people, the relationship between objective measures of sleep and “quality” sleep experience is not as strong as we might expect. And people with mild cognitive impairment may not be able to describe their sleep with this questionnaire as accurately as normal cognitive people because of memory loss and other cognitive difficulties. In addition, polysomnography monitors are expensive and labor-intensive, which are not suitable for use in large-sample epidemiological studies.
Conclusion
This large-scale survey of 1,443 villagers found that sleep disturbance is associated with MCI, especially for sleep duration, wake-up time, and habitual sleep efficiency. However, the causal relationships between sleep disturbances and cognitive impairment are not clear, which need to be further studied.